The 2026 CMS audit overhaul changed everything. If your healthcare organization is still running compliance off spreadsheets and quarterly checklists, you're already behind—and the financial exposure is real.
This isn't about being alarmist. It's about recognizing that the regulatory framework fundamentally shifted from a point-based scoring system to a zero-tolerance classification model. Every non-compliance finding now moves directly into remediation territory. There's no buffer. No wiggle room. No "we'll get to it next quarter."
The organizations that survive this transition are the ones that stopped treating compliance as a periodic event and started treating it as a continuous, autonomous process.
What Actually Changed in 2026
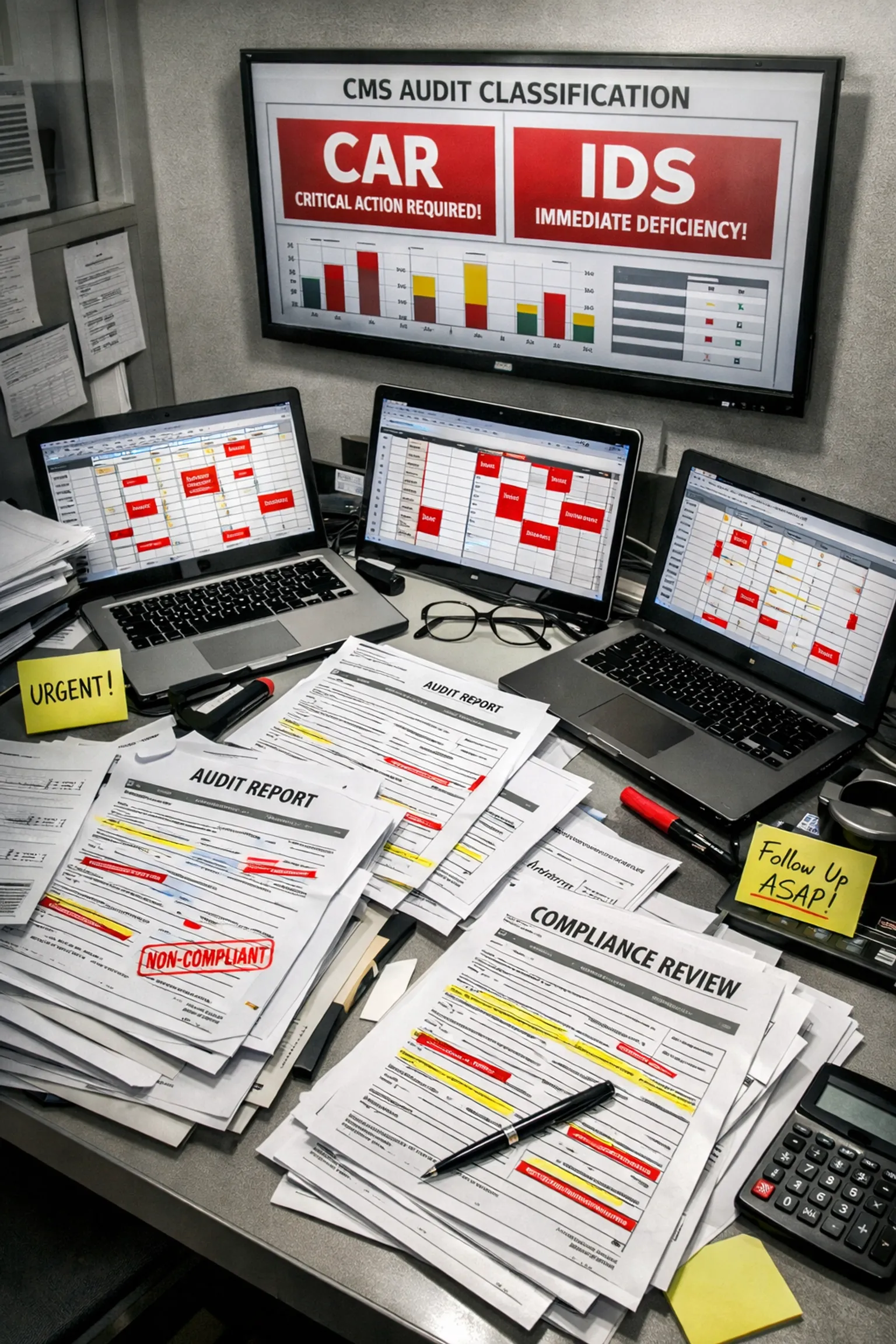
CMS eliminated audit scoring entirely. Instead, they introduced three classifications that healthcare executives need to understand cold:
Observation – Non-compliance that doesn't require corrective action (yet).
CAR (Corrective Action Required) – Non-compliance that triggers mandatory remediation with CMS oversight.
IDS (Invalid Data Submission) – Documentation or data universe failures that invalidate your entire submission.
The stakes escalated immediately. Without the old point system cushioning minor infractions, a single documentation gap can cascade into an IDS finding that puts your Medicare contracts at risk.
But here's the deeper issue: CMS isn't just auditing policies anymore. They're auditing Compliance Program Effectiveness (CPE)—the "how" of your operations. They want to see that your compliance activities are tagged with metadata capturing who did what, when, and why for every audit-relevant action.
Why Manual Checklists Can't Keep Up
Let's be blunt: if a compliance officer is manually checking boxes once a quarter, your organization is flying blind 90% of the year.
The old model looked like this:
- Quarterly audit prep scrambles
- Staff pulling reports from five different systems
- PDFs stacked in folders with vague naming conventions
- Post-it notes reminding someone to "check telehealth vendor compliance."
- Hope that nothing slips through the cracks
The new reality looks like this:
- Clinical coherence reviews that examine the entire patient care story in relation to billing patterns
- Real-time scrutiny of whether chronic diagnoses align with actual care management, follow-up timing, and medication adjustments
- Heightened telehealth compliance expectations, including cybersecurity controls and vendor oversight documentation
- Continuous data integrity validation across claims, appeals, enrollee data, and provider records
You can't manually keep pace with continuous monitoring. The human brain isn't wired to tag, trace, and cross-reference thousands of compliance touchpoints across multiple systems in real time.
What Autonomous Evidence Collection Actually Means
Autonomous evidence collection isn't about replacing your compliance team. It's about giving them a system that works 24/7 without babysitting.
Think of it as surveillance infrastructure for compliance. Instead of your team hunting for evidence after CMS sends an audit notice, the system is already capturing, tagging, and organizing evidence as clinical and administrative activities happen.
Here's how it works in practice:
Automated Data Tagging – Every billing submission, patient interaction, and provider note gets tagged with compliance-relevant metadata the moment it's created. No retroactive documentation hunts.
Cross-System Evidence Linking – When a claim is submitted, the autonomous system automatically verifies that supporting documentation exists across EHR, billing, and credentialing platforms. If something's missing, it flags it instantly—not six months later during an audit.
Continuous Compliance Monitoring – Instead of quarterly spot checks, the system runs real-time validation against HIPAA standards, CMS guidelines, and your organization's internal policies. It identifies drift before it becomes a CAR finding.
Audit Trail Transparency – When CMS asks, "How do you know this patient's chronic condition management aligns with the billed services?" your system doesn't just say "We documented it." It shows a timestamped, traceable chain of evidence from intake through follow-up.

The Metadata Imperative
CMS's focus on CPE means they're looking for operational proof, not policy statements.
It's not enough to have a documented policy that says, "We verify provider credentials every two years." CMS wants to see:
- Who verified credentials
- When the verification occurred
- What databases were checked
- How discrepancies were resolved
- Whether the verification happened on schedule or was delayed
This is where most healthcare organizations break down. They have policies. They have good intentions. But they don't have metadata infrastructure that captures compliance activities as they happen.
Autonomous systems solve this by embedding compliance into operational workflows. When a credentialing coordinator updates a provider profile, the system automatically logs the action with timestamps, user IDs, and change histories. When a nurse documents a telehealth encounter, the system validates that cybersecurity protocols were followed and logs the evidence.
The compliance team isn't chasing evidence. The evidence is self-generating.
Real-World Application: Telehealth Compliance
Telehealth exploded during the pandemic, and 2026 brought the regulatory reckoning. CMS now scrutinizes vendor oversight, data security standards, and clinical compliance documentation for every telehealth encounter.
Here's what manual compliance looks like for a mid-sized healthcare group handling 500 telehealth appointments a week:
- A compliance officer manually reviews vendor contracts quarterly
- IT staff running periodic security audits with no automated alerting
- Clinical staff documenting encounters in one system while compliance lives in another
- Cross-referencing telehealth billing with clinical documentation during audit prep
Here's what autonomous compliance looks like for the same organization:
- Vendor agreements are tagged with renewal dates and automatically flagged 90 days before expiration
- Cybersecurity controls are continuously validated against CMS standards, with instant alerts for configuration drift
- Every telehealth encounter is cross-checked in real time: Does the clinical note support the billed service? Was the patient's consent properly documented? Was the provider credentialed for telehealth in that state?
- Audit-ready evidence packages are generated on demand, pulling from a centralized, metadata-tagged repository
The difference isn't incremental. It's existential.

The IDS Risk Nobody's Talking About
Invalid Data Submission findings are the nuclear option in 2026 audits. When CMS determines that your data universe is inaccurate or incomplete, the entire submission is invalidated.
This happens when:
- Documentation exists, but isn't traceable to the source
- Data universes across claims, appeals, and provider records don't match
- The evidence is incomplete or contradictory
Manual systems are inherently vulnerable to IDS findings because they rely on humans to catch every discrepancy. Autonomous systems eliminate the risk by validating data integrity continuously rather than at submission time.
When a claim is generated, the system verifies that supporting documentation exists and matches across all relevant systems. If there's a mismatch—say, a chronic diagnosis code billed but no corresponding follow-up documentation—the system flags it before submission, not after CMS rejects it.
How to Implement Autonomous Evidence Collection
Most healthcare organizations approach compliance technology backwards. They buy a tool, then try to fit it into existing workflows. That's why adoption rates are abysmal, and compliance teams end up maintaining two systems—one automated, one manual.
The right approach starts with process mapping:
- Identify high-risk compliance touchpoints – Where are your IDS vulnerabilities? Which workflows generate the most audit findings?
- Centralize evidence repositories – Autonomous systems can't work if data lives in six different platforms with no API integration.
- Embed compliance into operational workflows – Don't bolt compliance on after the fact. Build it into how staff document encounters, submit claims, and manage provider credentials.
- Implement continuous monitoring dashboards – Compliance officers should see real-time metrics on documentation gaps, policy drift, and audit readiness—not wait for quarterly reports.
- Run internal mock audits using 2026 classification frameworks – Test your autonomous systems against actual CMS audit scenarios to identify blind spots before regulators do.
The goal isn't to replace your compliance team. It's to give them proactive intelligence instead of reactive firefighting.

The Exec Takeaway
Healthcare compliance in 2026 is no longer a quarterly event. It's a continuous operational discipline that requires autonomous infrastructure to execute at scale.
Organizations clinging to manual checklists are accepting catastrophic financial risk in exchange for familiar processes. The math doesn't work anymore.
Autonomous evidence collection isn't experimental. It's the baseline for surviving CMS audits in a zero-tolerance regulatory environment. The organizations that implement these systems now will spend 2026 focused on growth and patient care. The ones that wait will spend it in remediation.
If you're a healthcare executive or founder looking to build compliance systems that protect your organization 24/7 without constant human oversight, Bafmin specializes in autonomous AI solutions designed specifically for high-stakes regulatory environments.
The question isn't whether to implement autonomous evidence collection. It's whether you implement it before or after your next CMS audit.
